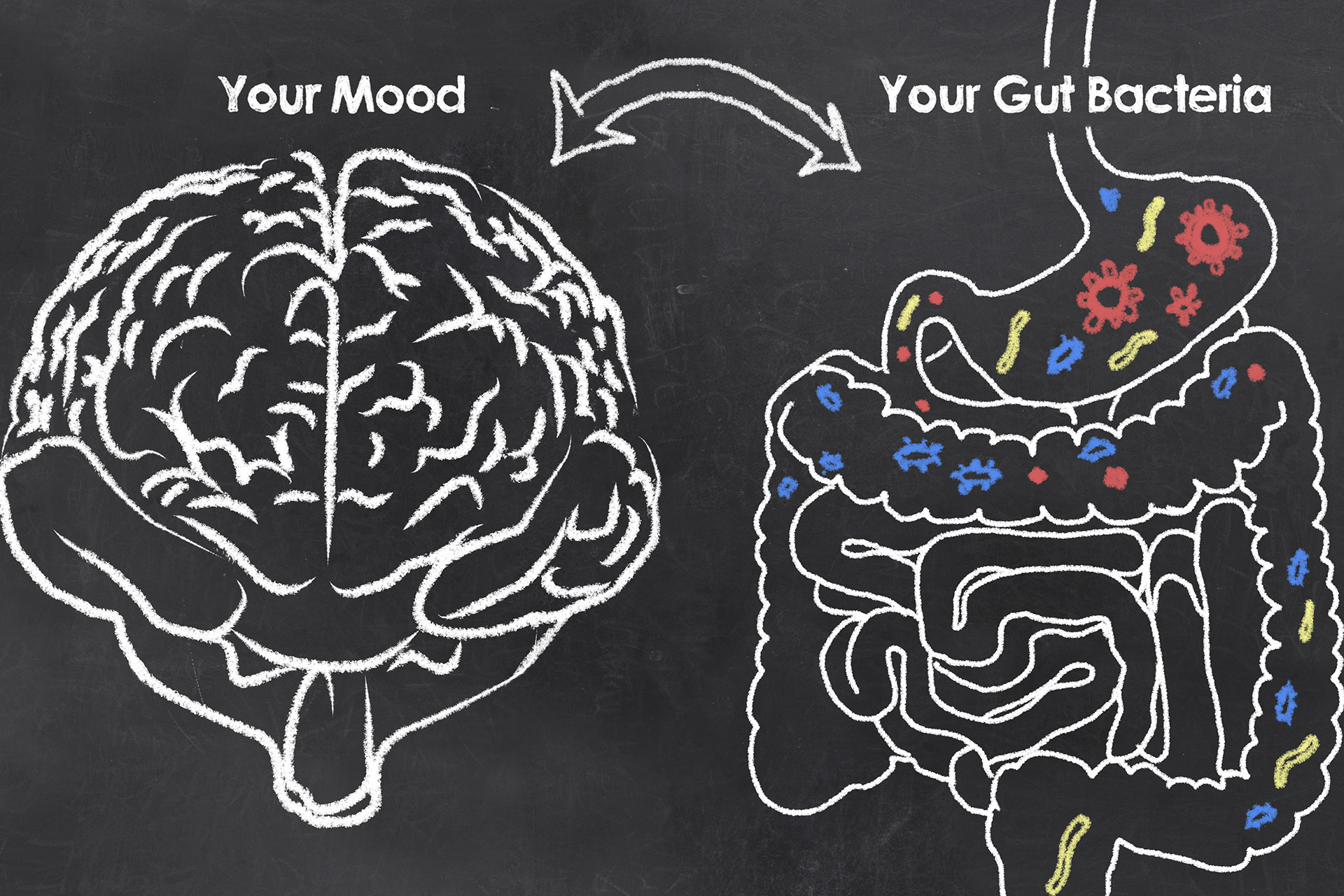
Understanding the axis that connects the intestine to the brain helps to understand how depression, anxiety, obesity, neurodegenerative diseases and autoimmune diseases are linked.
If you have lost your enthusiasm, if you are always anxious and are constantly overwhelmed by a wave of unbalanced emotions, relax. You are not a basket case. On the contrary, you are most likely part of an increasinggroup that suffers the consequences of the ”less than rosy” relationship between the gut and the brain.
It is not new that science knows that intestinal bacteria have receptors and produce neurotransmitters that enable direct communication with the brain via neural pathways, in exactly the same way as the vagus nerve works.
We can compare this process to a very complex and highly connective telephone line. This communication path between the intestine and the nervous system is called the “gut-brain axis” (GBA). Research has proven over and over again that changes in this system are directly linked to a number of diseases, such as depression, anxiety, gastrointestinal disorders, obesity, addictions, Alzheimer’s disease, Parkinson’s, multiple sclerosis and even cancer. Bingo!
This process was very well described by Emeran Mayer in his book The Mind-Intestine Connection. According to him, not only do intestinal microbeshave neurotransmitters that allow communication with the central nervous system (CNS), but they are also perfectly positioned in the gastrointestinal tract to receive information from the brain.
This means that even your, largely ignored, intestinal microbes understand wonderfully when you feel happy, stressed, anxious or angry, and immediately react accordingly. Your thinking starts in the brain, and generates a feeling or emotion that goes directly to your intestines. Did you feel it?
Therefore, the feeling that you would normally describe as “something inside me saying that something is wrong” is not just a figure of speech, but the perception of the huge involvement of your participatoryintestinal bacteria helping you to make decisions that you would classify as “intuitive”.
Isn’t this intelligence, that you can call a thousand different names, fascinating?
Of course, in this two-way relationship, just as mood influences and causes changes in intestinal bacteria, intestinal bacteria also interferes in moods. And all this directly impacts our extraordinary – and sotrendy – intestinal microbiome.
A healthy gut microbiome is seething with frantic bacteria that break down, absorb and assimilate nutrients from the food you eat, providing energy to all your body processes. But the work doesn’t stop there.
Now, for the best part: intestinal microbes also have another very important activity, which is to produce serotonin and dopamine, chemicals responsible for the “feeling good” sensation that helps to regulate and improve your mood.
The gut-brain interaction is so intense that approximately 90% of serotonin and 50% of dopamine are produced by the bacteria in your gut.
Therefore, when the gut is healthy, everything is peachy, so to speak. The communication lines with the brain flow perfectly. Serotonin is produced at adequate levels, signals of hunger and satiety are sent at the right time, nutrients are efficiently synthesized and so on.
As a result, you feel energized, calm and happy with life. This also helps to respond better to mental stress and to maintain a more balanced attitude. And that consistent, but unpretentious “happy-go-lucky” feeling is the best sign of good intestinal health.
However, not everything is harmonious in intestinal life. Certain habits and factors that are present in your diet, such as eating lots of sugar-rich foods,carbohydrates and/or hydrogenated fats, your lifestyle or continuous drug use often harm intestinal bacteria, suppress serotonin production and completely “alter” the communication between the intestine and the brain. These important changes in the microbiota considerably increase the chances of developing depression, chronic anxiety and other emotional disorders, as well as neurodegenerative and autoimmune diseases.
From now on, considering that you already know the impact of this axis within our physiology, choosing the right foods, not taking medicines unnecessarily and developing healthy lifestyle habits will be determinant factors for a long life – and most importantly, with quality!
References
- Gut-brain Axis: Role of Lipids in the Regulation of Inflammation, Pain and CNS Diseases. https://www.ncbi.nlm.nih.gov/pubmed/28215162
- Unhealthy gut, unhealthy brain: The role of the intestinal microbiota in neurodegenerative disease. https://www.ncbi.nlm.nih.gov/pubmed/30114473
- The Gut Microbiota and Alzheimer’s Disease. https://www.ncbi.nlm.nih.gov/pubmed/28372330
- Distinct Gut Microbiota Composition and Functional Category in Children With Cerebral Palsy and Epilepsy. https://www.frontiersin.org/articles/10.3389/fped.2019.00394/full